The current outbreak of novel coronavirus (COVID-19) was first reported as a cluster of pneumonia cases on Dec 31, 2019 from Wuhan, Hubei province, China. The WHO declared COVID-19 as a public health emergency of international concern (PHEIC) on Jan 30, 2020 and on 11th March 2020 WHO characterised the spread of coronavirus as a pandemic.
The spread of the virus can be monitored through various websites including the COVID-19 Global Cases by Johns Hopkins CSSE
This novel coronavirus route of transmission and clinical presentation is similar to SARS, with flu-like symptoms (typically involving fever, cough, shortness of breath) and acute respiratory failure (commonly bilateral pneumonia, acute respiratory distress). However, patients may present with atypical symptoms.
While COVID-19 has been suggested to have a lower case fatality rate (2.5%) than SARS (9.6%), MERS (34.4%), or H1N1 (17.4%), the extent of spread means that the death toll is significant. Frontline healthcare works are at most risk of becoming infected, and are also at risk of spreading infection. The Chinese National Health Commission acknowledged on Feb 14, 2020 that the infected medical workers in care of patients accounted for 3.8% of the total number of COVID-19 cases in mainland China.
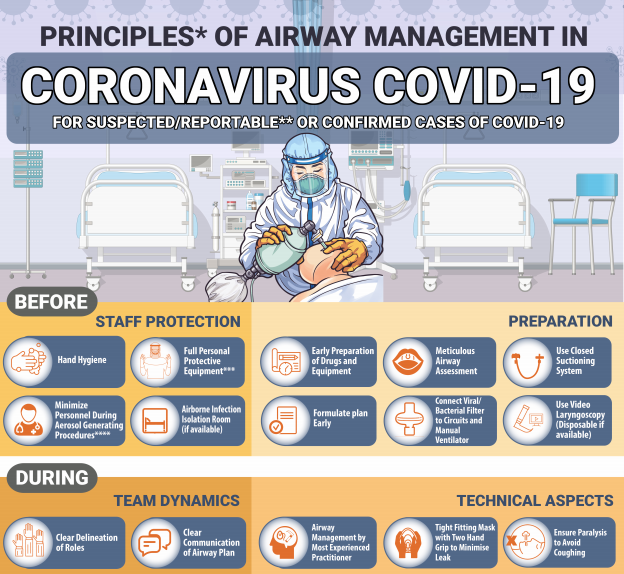
Anaesthesiologists and other perioperative care providers are particularly at risk when providing respiratory care and tracheal intubation of patients with COVID-19. WFSA would like to draw anesthesia team attention to the importance of appropriate precautions when providing respiratory care and intubation for these patients.
The following is intended as interim guidance for anaesthesia and perioperative care providers, largely derived from recommendations released by the Department of Anaesthesiology and Pain Medicine at the University of Toronto, and supported by a useful review published by Wax et al.
More extensive guidelines will follow shortly.
Routine Care for Patients with Suspected or Confirmed COVID-19
At a minimum, use droplet and contact precautions for suspected or confirmed cases of the 2019-nCoV. Some jurisdictions are recommending routine use of airborne, droplet and contact precautions (including an isolation room appropriate for airborne infection isolation) for suspected or confirmed cases of the 2019-nCoV. However, triage for airborne precautions and isolation rooms will necessarily be based on level of suspicion, and types of procedures provided, and available facilities. All healthcare providers should be trained in infection control and prevention strategies, and in procedures for donning and doffing personal protective equipment (PPE). Healthcare facilities should provide healthcare workers with adequate PPE isolation facilities to meet the requirements for airborne, droplet and contact precautions. Practice appropriate hand hygiene before and after all procedures. Patient rooms with suspected or confirmed COVID-19 should be labelled with a sign, so that all healthcare workers and support staff are aware of the risk before entering the area.
High Risk Procedures – Intubation and other Aerosol-generating medical procedures (AGMP)*
Protecting healthcare providers is the first priority, as you are the primary line of defense for this patient, and upcoming patients. Ensure adequate time for reviewing the intubation plan, and for donning PPE. Preferably prepare a checklist to guide the procedure. Enhanced PPE is required for AGMPs. A fit-tested N95 respirator (or powered air purifying respirator (PAPR) device, if one is adequately trained to use), face shield, gown, and double gloves (preferably long gloves). Minimize the number of staff in the room to the number required to provide safe intubation. Preferably, the most experienced anaesthesiologist should perform the intubation. Before the procedure begins, ensure all equipment is ready: standard monitoring equipment, i.v. access, drugs. Ensure ventilator and suction equipment is functional. Avoid awake fiberoptic intubation (due to risk of coughing and aerosols). Consider videolaryngoscopy to minimize close exposure between anaesthesiologist and patient respiratory aerosols. Plan for rapid sequence induction (RSI). RSI may need to be modified to ultra-rapid, if patient has very high alveolar-arterial gradient and is unable to tolerate a short period of apnoea, or has a contraindication to neuromuscular blockade. If manual ventilation is required, apply small tidal volumes only. Five minutes of preoxygenation with oxygen 100% and RSI in order to avoid manual ventilation and potential aerosolization of infectious respiratory droplets. Ensure high efficiency hydrophobic filter placed between facemask and breathing circuit or between facemask and Laerdal bag. Intubate and confirm correct position of tracheal tube. Institute mechanical ventilation and stabilize patient. The use of high-flow nasal oxygenation and mask CPAP or BiPAP should be avoided due to greater risk of aerosol generation. All airway equipment must be decontaminated and disinfected according to appropriate hospital and manufacturer policies. Ensure all dirty equipment is placed in a bin that is appropriately labelled for the support staff who collect and process the equipment. Remove outer gloves before touching any spaces that may be touched by others. Doff equipment within an area designated for doffing dirty PPE. After removing protective equipment, avoid touching hair or face before washing hands. Practice hand hygiene before and after all procedures.
*aerosol generating procedures include intubation, extubation, bronchoscopy, airway suction, high frequency oscillatory ventilation, tracheostomy, chest physiotherapy, nebulizer treatment. These procedures should be performed in the COVID-19 patient only when the benefits outweigh the risks, and when adequate PPE and staff preparation is available.
Additional guidance on Coronavirus and anaesthesia
- APSF – Perioperative Considerations for the 2019 Novel Coronavirus (COVID-19)
- SIAARTI – Covid 19 – Airway Management
- Prince of Wales, Hong Kong – Principles of Airway Management in Coronavirus
- RCoA, The Faculty of Intensive Care Medicine, the Intensive Care Society and the Association of Anaesthetists. – Obstetric anaesthesia guidance
- ASA – Coronavirus (2019-nCoV)
- SBA – Recomendações Coronavírus
- SCARE – ¿Qué recomendaciones hay que seguir con pacientes que tengan una infección respiratoria aguda severa?
Coronavirus – General Information
- WHO – Coronavirus disease (COVID-19) outbreak
- WHO – Novel coronavirus (2019-nCoV)
- WHO – Emerging respiratory viruses, including nCov: methods for detection, prevention, response and control
- WHO – Online training as a weapon to fight the new coronavirus
- CDC – Information for Healthcare Professionals
- MSF – MSF update on novel coronavirus outbreak
- WHO – Report of the WHO-China Joint Mission on Coronavirus Disease 2019 (COVID-19)